INTRODUCTION
Leadership in healthcare setting continues to receive overwhelming attention from management researchers, policy makers and the multiple healthcare professional groups.[1,2] This level of curiosity is by and large in the UK’s National Health Service (NHS) where a series of initiatives have demonstrated organisational improvement and clinical effectiveness by concentrating on the type, responsibility and attribution of leaders and leadership.[3] Furthermore, Darzi[4] recommendations have led to a multiple number of leadership interests and institutionalised initiatives such as NHS Leadership Academy in England, funding support for clinical leadership research and multiple reports on leadership from the Kings Fund, Health Foundation, and professional societies.[5,6,7] However, it can be argued these initiatives are driven by perception of failings in service provision and their solutions can be ascribed to leadership deficiency.[8]
The purpose of this article is to critically discuss, distributed leadership and its integral role as the potential solution to the above perceived leadership problem. The paper will conclude by summarising a case study, highlighting the usefulness and application of distributed leadership in driving innovation and transformation on a large-scale.
Leadership styles such as transformational leadership inspires followers to meet their collective goals[9] and transactional is more centric on supervision and performance (Mullen & Cooper, 1994) are complimentary as formal leaders play a pivotal role in distributing leadership within the organisation.[10] Distributed leadership (DL) stems from Gronn’s[11] and Jonsson’s[12] agency approach and can be described as allocation of collective leadership assignment to persuade resource availability, decision making and setting objectives within the organisational context.
The concept of distributed leadership aims to empower experts in the ecosystem thereby addressing some of the criticisms of conventional leadership which have tendencies to centralise power at the top of the organization.[13]
Brookes and Grint,[14] suggest that distributed leadership’s main intentions are engagement and empower ment, subsequently resulting in a vertical flow of power from the centre bottomwards, and most likely outside the borders of the organisation. Numerous studies sug gest that DL increases staff job satisfaction and involvement in addition to professional and organisation empowerment.[15,16] Furthermore, distributed leadership can subsequently result in raised organisational effectiveness.[17]
Therefore, it can be argued that power should be more evenly distributed than in folkloric hierarchical structure and staff at various levels of the ecosystem should be empowered in decision making and execute them in a concerting fashion.[18,19] The emerging distributed leadership role pause a paradox “What is the role formal leaders when staff take on leadership impetuously as demonstrated in distributed leadership?” Leaders are still required as they play an important role in distributing leadership across different employees of the organisation.[20] Additionally, formal leaders promote organisational culture enabling distributed leadership to spread out. Therefore, the various leadership styles for example transformation, transactional and empowering play a role on employees’ participation in distributed leadership practices.
DISTRIBUTED LEADERSHIP IN HEALTHCARE
The healthcare industry is dependent on expert reasoning of hierarchy which promotes top-down approach and leadership.[11] This makes distributed leadership style relevant to those formal leaders in organisations. In some reports, distributed leadership is described in a more structural approach where leadership roles and responsibilities are delegated to clinical departments and teams working at operational levels. In the NHS, there has been the introduction of the competency framework, demonstrating the leadership roles agenda in which medical staff and other clinical staff are expected to be involved. Furthermore, the King’s Fund has advocated for distributed leadership to clinicians acknowledging the importance of incorporating expert knowledge into leadership in the wider healthcare ecosystem.
The figure below summarized distributed leadership as collective, distributed activity, constructed through interaction, and involving managers operating at different levels, both within traditional organizational boundaries, as well as managers operating in more networked forms of service delivery. (Figure 1)
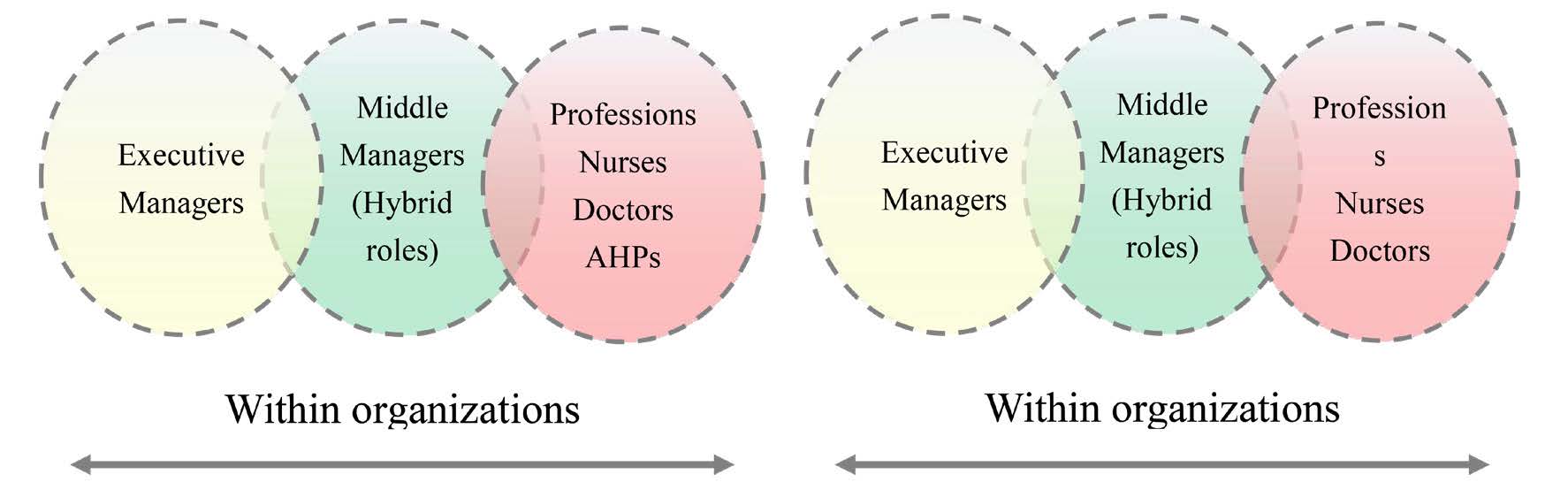 Figure 1: Across organizations[18,21]. Presented by Crump B Warwick Business School slides presented January 2022 at the Strategic Leadership for the Healthcare Industry MBA Elective Module (Permission sought from the Lecturer).
Figure 1: Across organizations[18,21]. Presented by Crump B Warwick Business School slides presented January 2022 at the Strategic Leadership for the Healthcare Industry MBA Elective Module (Permission sought from the Lecturer).
The above illustration can be applied in patient care delivery. For example, the capacity for the organisation to deliver seamless patient care and high-quality therapy is not dependent on a single leader, rather, leadership input from clinicians delivering care, middle managers supporting clinicians and executives as formal leaders and driving strategy. The multi-disciplinary requirements of most patient processes demand full cooperation between departments and the ability to charismatically distribute and designate decision making among the staff. Furthermore, to achieve patient experience and safety outcome, clinical staff need to share similar strategic objectives and organisational values with the executives and managers.[22]
There are variants of distributed leadership with a close link to concepts such as shared leadership,[23] team leadership and “followership”.[24] Whilst there are overlaps amongst these concepts of leadership, this does not suggest that all types are equal or assume that everyone is a leader.[25]
OPHTHALMOLOGY CASE STUDY AND DISTRIBUTED LEADERSHIP
Contextual background
Increasing ageing populations subsequently lead to increase in prevalence of age-related macular degeneration, rise in diabetes and incidence of diabetic macular oedema. These remain the two leading disease spectrum causes of visual loss globally.[26,27] The discovery of ANTI-VEGF in 2006 was described as research breakthrough in the treatment of both age-related macular degeneration and diabetic macular oedema.
However, the monstrous resources, rising costs and huge efforts of viable intravitreal therapy delivery have placed enormous burden on both service providers and users.[28] When the injections were licensed in the UK, there were fewer ophthalmologists to deliver sight saving therapies and meet growing demands for patients waiting treatments. In the UK it is estimated that there are approximately 7000 new cases of wet age-related macular degeneration per year. The small pool of ophthalmologist’s resources could not meet the demands characterised by long waiting lists resulting in exponential burden in the eye clinic department. Furthermore, ophthalmology was increasingly faced with growing number of outpatient appointments.
Distributed leadership and nurse delivered injection implementation
Transformational leadership is highly regarded as one of the most prominent modern leadership theories, in eloquently setting a compelling vision such as nurse led injection. However, the author feels distributed leadership played an integral role for the success of this project. Through distributed leadership across the department, clinicians, middle management and senior executives, nurse delivered intravitreal injection was implemented in 2012. This followed a lengthy process of engagement with various stakeholders both externally and internally to the organisation. The initial step was to acknowledge the problem and identify remedial measures to address the growing crisis in the medical retina service. The author in collaboration with medical leads, approached senior management with business case outlining the challenges and opportunities in implementing nurse led injection. The business case put in place can be summarised below with the application of the strengths, weaknesses, opportunities, threats (SWOT) analysis.
Below is Figure 2 illustrating the SWOT analysis for the implementation of a Nurse-led intravitreal injection service.
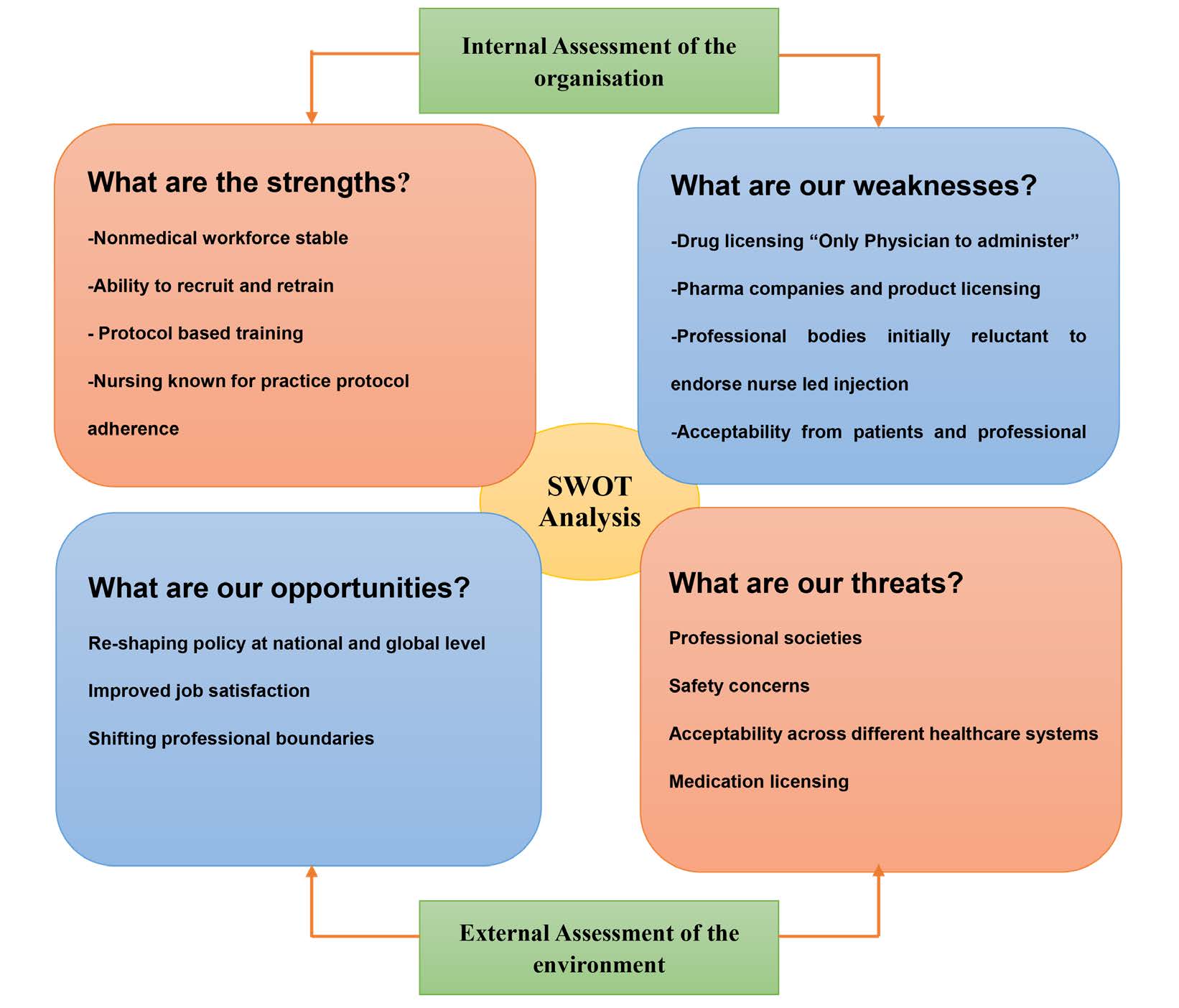 Figure 2: SWOT analysis for the implementation of nurse-led intravitreal injection. SWOT: strengths, weaknesses, opportunities, threats.
Figure 2: SWOT analysis for the implementation of nurse-led intravitreal injection. SWOT: strengths, weaknesses, opportunities, threats.
Following a lengthy discussion and approval process, the trust management executive finally gave approval for nurse led injections. This included the establishment of policy documents, legal process involvement, engagement with cooperate governance department, patient, and professional societies. (Figure 3)
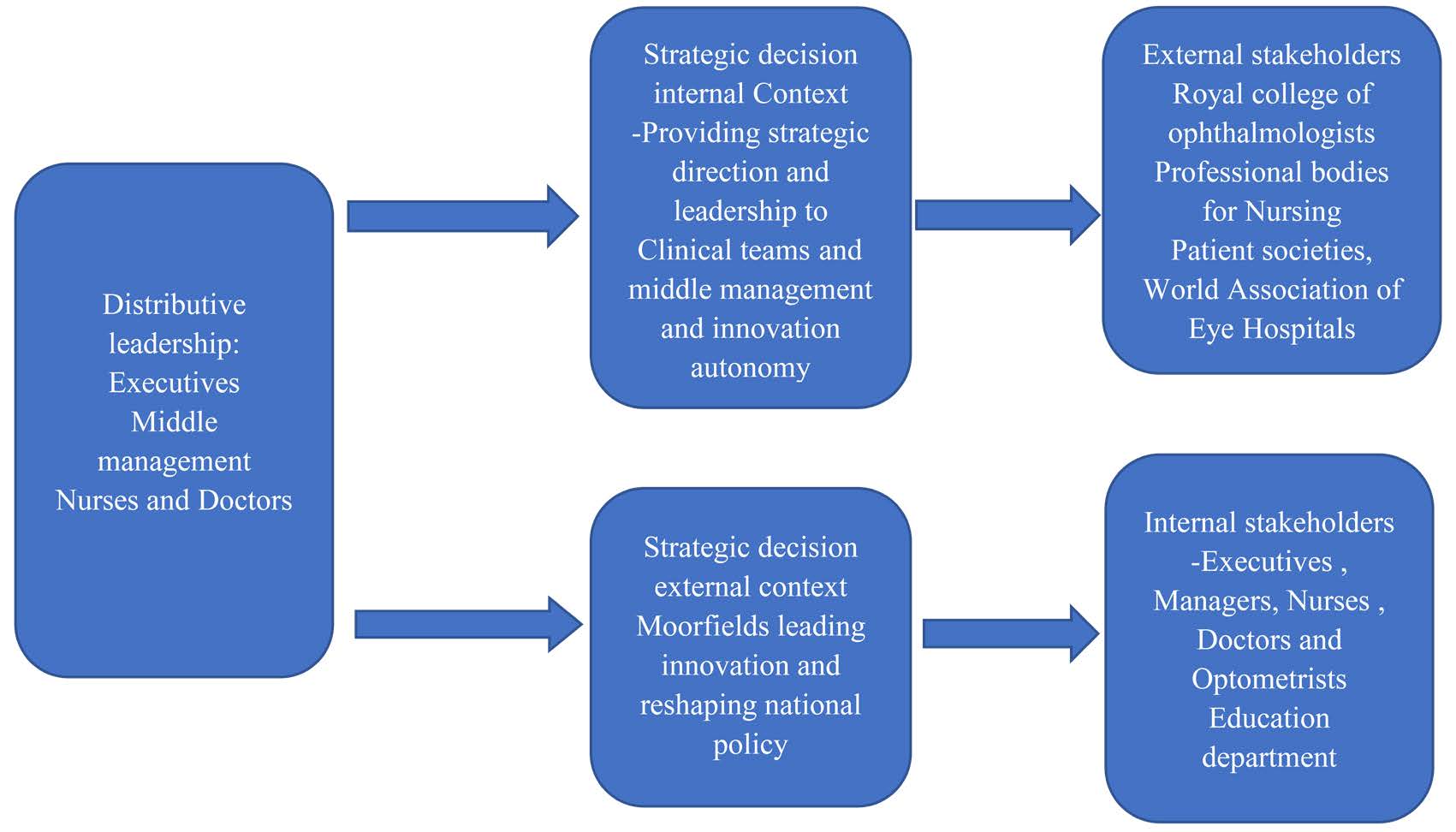 Figure 3: Illustration of distributed leadership in the implementation of nurse led injection.
Figure 3: Illustration of distributed leadership in the implementation of nurse led injection.
Organisational efficacy and distributed leadership
The nurse-led injection practice at Moorfields led to excellent safety outcomes and improved patient experience, which were presented at the World Association of Eye Hospitals in Seoul, South Korea (2012). Following the successful implementation of the nurse led injection service, the author received multiples of enquiries both nationally and internationally on how the service was set up and the impact on patient care. An intravitreal injection course was established in some form of distributed leadership involving University College London academic partner, nurse practitioners, managers, and legal advisors. The course was designed to showcase the success of our innovation, what had been accomplished, how they were accomplished and how they could be applied in practice.
Followership to leadership
Leadership studies have been focused on leaders, whereas there is limited understanding and studies on followership.[29] Re-shaping and influencing policy non-medical delivery of injections prompted the need to turn large follower- practitioners to become leaders in the delivery of injections. Transformational leadership style was applied to individual followers’ transformation process, in setting up their own independent non-medical injection services.[30] The nature of the large-scale project required distributed leadership including consultant ophthalmologists’ local leads, business managers, industry partners and professional societies. Internationally, there was a growing call for distributed leadership in different global healthcare systems, different from the UK’s NHS Beveridge model.
The author presented the first ever patient safety and satisfaction outcome of Nurse led intravitreal injection at the Association for Vision Research in Ophthalmology (ARVO) global meeting in 2016 Seattle USA. Furthermore, there were requests to present at other international and national symposia. Having trained more than 1300 practitioners so far, the course has become a global brand, reaching out to Singapore, Australia, United States, South Africa, Europe, Hong Kong, and New Zealand. The author is in frequent demand to present and share knowledge on service transformation and innovation at national and international symposiums.
The author acknowledges the role of other leadership styles such as empowering, transformational, and transactional in supporting the employee agency of distributed leadership. Additionally empowering leadership would perpetuate the success of this story, by enabling staff to gain confidence in leading discussions and across organisational hierarchy. Furthermore, the essential of overall for mal leadership in the context of such large-scale change is acknowledged. The role played by formal leaders was so integral role in inspiring, enabling transformation and success of the vision in line with organisational strategy. However, the current Volatile Uncertainty Complex Ambiguity (VUCA) world environment empathetical leadership has demonstrated its efficacy in responding to the corona virus disease 2019 (COVID-19) crisis.
CONCLUSION
This paper discusses the significance of distributed leadership in healthcare and impact on service transformation. The concept of distributed leadership is explored in the context of healthcare sector where hierarchical structures are traditionally established. Leadership may have positive impact on the spread of distributed leadership. Despite their leadership style, formal leaders play a significant role in inspiring, engaging, motivating, and inaugurating members of staff to adopt leadership tasks. Distributed leadership requires time to establish relations, dialogue and negotiations in order to achieve intended outcomes. Furthermore, distributed leadership calls for preparedness amongst stakeholders and the need for change in organisational culture.
DECLARATIONS
Acknowledgments
Thank you: Professor Bernard Cr ump – Professor of Practice with a Healthcare Special interest; Ms. Louisa Wickham -Consultant Ophthalmic Surgeon and Moorfields Eye Hospital Medical Director; Mr. Robin Hamilton -Consultant Ophthalmic Surgeon and Service Director Medical Retina Moorfields; Professor David Probert, University College London Hospital Chief Executive Officer; Moorfields Medical Retina Nursing, Management, Medical and Optometry Teams Moorfields Eye Hospital.
Source of Funding
None.
Conflict of Interest
The authors declare no conflict of interest.
REFERENCES
- Degeling P, Zhang K, Coyle B, Xu L, Meng Q, Qu J, et al. Clinicians and the governance of hospitals: a cross-cultural perspective on relations between profession and management.
Soc Sci Med 2006;63:757-775. DOI: 10.1016/j.socscimed.2006.01.034 PMID: 16580109 - Kirkpatrick I, Jespersen PK, Dent M, Neogy I. Medicine and management in a comparative perspective: the case of Denmark and England.
Sociol Health Illn 2009;31:642-658. DOI: 10.1111/j.1467-9566.2009.01157.x PMID: 19392937 - Martin G, Beech N, MacIntosh R, Bushfield S. Potential challenges facing distributed leadership in health care: evidence from the UK National Health Service.
Sociol Health Illn 2015;37:14-29. DOI: 10.1111/1467-9566.12171 PMID: 25529349 - Darzi L. High Quality Care for All: NHS Next Stage Review, Final Report. London: Department for Health, 2008.
- National Health Service (NHS) Leadership Academy. The leadership framework. Warwick: NHS Institute for Innovation and Improvement. 2011. Available at: http://www.leadershipacademy.nhs.uk/wp-content/uploads/2012/11/NHSLeadership-Leadership-Framework-Clinical-Leadership-Competency-Framework-work-CLCF.pdf. Accessed February 20, 2022.
- NHS Institute for Innovation and Improvement. Shared Leadership: underpinning of the medical leadership competency framework. London: Academy of Medical Royal Colleges. 2009. Available at: https://www.fmlm.ac.uk/resources/shared-leadership-underpinning-of-the-mlcf. Accessed February 20, 2022.
- O’Relly D, Reed M. Leaderism:an evolution of managerialism in UK public service reform.
Public Administration 2010;88:960-978. - Storey J, Holti R. Possibilities and Pitfalls for Clinical Leadership in Improving Service Quality, Innovation and Productivity. Final Report. NIHR Service Delivery and Organisation Programme. London: HMSO, 2013.
- Bass MB. Leadership and performance beyond expectations. New York: The Free Press, 1985.
- Gronn P. Hybrid Leadership. In Leithwood, K., Mascali, B. and Strauss, T. (eds) Distributed leadership According to the Evidence. Abingdon: Routledge, 2009.
- Bate P. Changing the culture of a hospital: from hierarchy to networked community.
Public Adminstration 2000;78:485-512. - Jonsson T, Unterrainer C, Jeppesen HJ, Jain AK. Measuring distributed leadership agency in a hospital context: Development and validation of a new scale.
JOM 2016;30:908-926. DOI: 10.1108/JHOM-05-2015-0068 PMID: 27681024 - Fitzsimmons D, James K T, Denyer D. Alternative approaches for studying shared and distributed leadership.
International Journal of Management Reviews 2011;13:313-328. - Brookes S, Grint K. The New Leadership Challenge. Basingstoke: Palgrave MacMillan, 2010.
- Day DV, Gronn P, Salas E. Leadership in team-based organisations: on the threshold of a new era.
Leadership Quarterly 2006;17:211-216. - Leithwood K, Mascall B, Strauss T. Distributed Leadership According to the Evidence. London: Routledge, 2009.
- Hulpia H, Devos G. Development and validation of scores on the distributed Leadership Inventory.
EPM 2009;69:1013-1034. - Currie G, Lockett A. Distributing leadership in Health and Social Care: Concertive, conjoint or collective?
Int J Manage Rev 2011;13:286-300. - Groon P. Distributed leadership In Leithwood K and Hallinger P(eds) Second International Handbook of Educational leadership and Administration. Dorderecht: Kluwer, 2002.
- Gronn P. The Future of distributed leadership.
Journal of Educational Administration 2008;46:141-158. - Denis J, Langley A, Sergi V. Leadership in the Plural.
The Academy of management Annals 2012;6:211-283. - Gittell JH. Coordinating mechanisms in care provider groups: relational coordination as a mediator and input uncertainty as a moderator of performance effects.
Management Science 2002;48:1408-1426. - Pearce CL, Conger JA. Leaderish: Shared leadership: Reframing the How’s and Whys of Leadership. Thousand Oaks: Sage, 2003.
- Bligh MC. Followership and Follower-Centred Approaches. Sage Handbook of Leadership. Thousand Oaks: SAGE Publications Ltd, 2010.
- Leithwood K, Day C, Sam mons P. Successful School Leadership: What It Is and How It Influences Pupil Learning. Nottingham: Dfes Publications, 2006.
- Wong WL, Su X, Li X. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis.
Lancet Glob Health 2014;2:e106- 116. DOI: 10.1016/S2214-109X(13)70145-1 PMID: 25104651 - Yau JW, Rogers SL. Kawasaki R. Global prevalence and major risk factors of diabetic retinopathy.
Diabetes Care 2012;35:556-564. DOI: 10.2337/dc11-1909 PMID: 22301125 - Spooner KL, Mhlanga CT, Hong TH, Broadhead GK, Chang AA. (2018). The burden of neovascular age-related macular degeneration: a patient’s perspectives.
Clin Ophthalmol 2018;12:2483-2491. DOI: 10.2147/OPTH.S185052 PMID: 30584267 - Hollander EP. Essential interdependence of leadership and followership.
CDPS 1992;1:71-75. - Bryman A. Charisma and leadership in organizations. London: SAGE Publications Ltd, 1992.