Diagnostic and therapeutic care pathways of cancer patients: A model of multidisciplinary management and patient-tailored healthcare at University Hospital in Italy
Veronica Agostinelli1#, Valeria Cognigni1#, Valentina Lunerti1, Camilla Cicoli1, Giulia Ricci1, Roberto Papa2, Michele Caporossi3, Rossana Berardi1*
1Department of Medical Oncology, Università Politecnica delle Marche, AOU Ospedali Riuniti Di Ancona, Ancona 60126, Italy
2Quality, Risk Management and Heath Technolog y Innovation Unit, Department of staff, AOU Ospedali Riuniti Ancona, Ancona 60126, Italy
3General Direction, AOU Ospedali Riuniti of Ancona, Ancona 60126, Italy
Corresponding author:
Rossana Berardi, E-mail: r.berardi@staff.univpm.it
For reprints contact: reprints@sppub.org
Received 01 April 2022; Accepted 04 August 2022; Available online 28 September 2022
INTRODUCTION
Recently cancer patients’ therapeutic needs have been drastically changed due to the population growth, the increasing life expectancy and the technological progress. Advances in cancer prevention, diagnosis and treatment have led to reduced cancer mortality rates and increased 5-year survival after diagnosis.[1]
Many therapeutic strategies have changed the approach to oncology in recent decades: immunotherapies and targeted therapies have brought a real revolution for advanced tumours, improving patient’s survival and quality of life. The goal of cancer treatment strategies and clinical research is to make the oncological disease chronic and to customise care pathways for each patient. Better management of patients with complex disease, which increasingly requires multidisciplinary management, has resulted in improvement of survival by means of a personalised approach based on the specific characteristics of the disease.[2]
The employment of a multidisciplinary approach has become more significant both within the diagnostic and therapeutic settings, ensuring improved awareness and continuity of patient care.[3,4,5]
Therefore, in Italy the establishment of the so called Diagnostic Therapeutic and Care Pathway (PDTA) including the adoption of the multidisciplinarity requirement has emerged in hospitals.
PDTA refers to a clinical pathway aimed to the care of specific groups of patients, through the coordination and implementation of standardised sequential activities by a multidisciplinary team of experts and based on latest scientific evidences.[5] The aim is to improve the efficiency of care guaranteeing an equal access to care to as many patients as possible. Furthermore, PDTA allows developing diagnostic and therapeutic management, to reduce the treatment start time and to guarantee patient care by expert, dedicated and qualified personnel.
PDTA summarises a patient’s path through several health organisations and provides the optimum sequence of activities required to attain the defined health objectives. In the systemic vision of care, the PDTA allows the overcoming of individual ser vices, embracing the model of an individualised and personalised care on the patient.[6,7]
In recent decades, biotechnological development has progressively led to the identification of gene expression abnormalities associated with carcinogenesis that is reflected in specific biological features and may be targeted by specific treatments. In the last period, the evolution of techniques based on genomics, proteomics and metabolomics has been increasingly taking place.[8]
Tissue and serological biomarker analysis, including genomic technologies, has allowed to conceive the concept of precision oncology, that is actually essential for treatment decisions. Therefore, clinical trials are progressively shifting from tumour type-focused research to gene-oriented research with innovative design adapted to the biomarker profile.[9]
In this context, recent clinical protocols based on innovative targeted drugs use have been progressively developed. The technological advancement of gene sequencing techniques, the reduction of costs and the increase in the number of targeted therapies led us to apply in clinical practice innovative high-processing technologies, such as next generation sequencing (NGS).
Clinicians will therefore be faced with more and more complex genetic information and this novel comprehensive knowledge about molecular findings will represent a major challenge for oncologists to guide the therapeutic choice. A multidisciplinary management will be required integrating teams from oncology, haematology, molecular biology, pathology, hospital pharmacy and genomic experts in order to govern the clinical care processes appropriately. The multidisciplinary Molecular tumour board (MTB) was created to bridge this gap and to share experiences when literature evidences are limited or when there are no guidelines or defined quality criteria. Teams of experts joined by MTB aim to manage cancer patients’ complexity and to deeply interpret genomic profiling tests, by helping colleagues choose the best treatment option and access to active drugs (or combinations) studied in clinical trials.
GOALS
This manuscript aims to describe the organisational model of the Department of Oncology at the University Hospital of Ancona (“Azienda Ospedaliero-Universitaria, AOU, Ospedali Riuniti Ancona - Università Politecnica delle Marche”, Italy), focusing on main aspects:
- importance of the multidisciplinary approach in the management of patients.
- application of precision medicine to establish the best treatment strategy personalised to each individual patient.
- local experience in developing PDTA, especially focusing on our Breast Unit model.
- local experience in the context of the MTB.
DISCUSSION
The AOU Ospedali Riuniti di Ancona is located in the regional capital of Marche region and represents the reference hospital for the whole regional territory, constituting a highly specialised and high-volume unit (Figure 1). In this context, the Department of Oncology aims to create an innovative diagnostic, therapeutic and care model that can be taken as an example from different territorial entities.

Figure 1: Location of AOU Ospedali Riuniti di Ancona, reference hospital of Marche Region.
CORM (cancer and research center of marche – centro oncologico e di ricerca delle marche)
The AOU Ospedali Riuniti di Ancona has been considered as the most suitable institution to host the Cancer Center, due to its leading role as a highly specialised hospital and given its integrated reality with the Università Politecnica delle Marche. cancer and research center of marche(CORM) was established at the Department of Oncology of the AOU Ospedali Riuniti di Ancona under the patronage of the Ministry of Health in April 2021. The project was born with the need to create a close connection among physicians of all the Hospitals of Marche region and territorial medicine, with the primary goal of guaranteeing cancer patients the best diagnostic, therapeutic and care pathway.
The main objectives of CORM include:
- Promotion and consolidation of the regional oncology network, with the aim to fully achieve the Essential Levels of Care in the oncologic area.
- Support of the development of all health service instances in the field of territorial and hospital prevention.
- Encouragement and development of clinical and translational research, including phase I trials with innovative drugs that require an Italian Regulator y Agency of Drugs (AIFA) accreditation. This accreditation has already been obtained by the Department of Oncology of AOU Ospedali Riuniti di Ancona which is the only one active Phase I Center in Marche region and in central Italy at the current time.
- Promotion and development of research in oncological genetics for hereditary tumours being the Highly Specialised Regional Reference Center afferent to the Departmen of Oncology, too, for the benefit of all the regional Hospitals.
- Promotion and consolidation of cancer diagnostic and therapeutic pathways, with particular regard to neoplasms that require a collaborative and multidisciplinary management.
- Promotion of the regional operational model of PDTA.
The CORM Cancer Center is placed in the context of a regional Comprehensive Cancer Center Network.
The CORM achieves its goals and is effectively active through:
- Highly experienced teams of professionals.
- Interdisciplinary expertise.
- Pathology-specific pathways and personalised therapies.
- Patient facilities.
- State-of-the-art technologies.
- Clinical, translational and basic research.
- Close collaboration with international cancer centers.
Major projects of CORM include:
- An informatic infrastructure with dedicated website and platform for telemedicine, that allows connection with other Hospitals and general practitioners. (www.corm-marche.it)
- The MTB, a multidisciplinary group aimed to translate complex molecular information into data that can be used by clinicians for prognostic purposes and as a predictive tool for cancer treatment efficacy.
- Artificial intelligence projects, which analyse the huge amount of clinical and molecular data derived from the MTB and from research projects.
- Clinical trials, including early phase trials, which allow us to offer cancer patients from the entire Marche region and beyond new therapeutic opportunities.
- Communication and dissemination projects also through social networks to provide patients, caregivers and associations with easily accessible information.
- High specialized Regional Center in Oncological Genetics, already active at Ospedali Riuniti di Ancona since 2004. The goal is to offer genetic counselling in the field of oncology to individuals (and their families) who are at increased risk of cancer due to a genetic predisposition on hereditary basis.
Diagnostic, therapeutic and care pathway (PDTA)
AOU Ospedali Riuniti di Ancona is a structure that, over the years, has designed countless PDTA, guar anteeing professionals and patients top quality pathways. On September 14, 2018 it obtained the certification of compliance with ISO 9001/2015 regarding clinical care pathways and it was the first one in Italy to certify the entire organisation for PDTA and not only for individual ser vices (pathway certified by the Quality Management System-ITALCERT).
The Department of Oncology includes a team of experienced professionals, with interdisciplinary expertise and it has organised over time specific therapeutic pathways, including taking charge for different solid cancer types.
Breast unit as a model of PDTA
Many scientific studies have shown that the prognosis of breast cancer patients improves dramatically if a multidisciplinary team made up of experienced specialists operating in high volume centers manages the diagnostic and therapeutic pathway.[4,10,11]
According to the latest evidences, Breast Units have been established in the hospitals to support breast cancer patients from the beginning of the disease and through all oncological treatments, whethever surgical, radiation or medical ones. The Breast Unit active at Ospedali Riuniti di Ancona makes use of a tested and dedicated PDTA, made up of professionals who collaborate for the diagnosis and the best treatment of breast cancer patients.
Each week, the reference specialists of the Breast Unit meet to discuss the clinical cases and to define, collectively, the diagnostic and therapeutic path of each patient, personalising the treatment pathway and reducing the start time of the best specific treatment identified.
The Breast Unit Core team consists of:
- Department of Breast Surgery, high-volume specialised breast surgery center. It consists of a group of experienced breast surgeons who are able to offer the best treatment approach, with an activity of more than 600 surgical interventionals for breast cancer.
- Department of Radiology, made up of dedicated radiologists and experts in breast diagnostics, with a volume of more than 22,000 radiological exams (mammography, ultrasound and MRI) for breast cancer patients.
- Nuclear Medicine, whose role is fundamental during diagnosis to set the correct surgical approach and in the staging process.
- Pathologic Anatomy that has, within itself, simple units of Diagnostic Cytopathology and Molecular Biology and that include an expert team in the management of breast cancer.
- Two Departments of Plastic and reconstructive surgery, with an experienced and dedicated team of surgeons, able to offer the best and innovative techniques of plastic and reconstructive surgery.
- The Department of Oncology, including medical oncologists dedicated to the management of patients affected by breast cancer.
- Radiation Oncology, a specialised center endowed of latest equipment and technologies. It is composed of experienced and dedicated staff who actively participates in treatment of breast cancer by supervising many working groups such as the one dedicated to the development of guidelines.
- Two Departments Neurorehabilitation, in which dedicated professionals carry out activities of prevention and treatment of impairments and disabilities emerging in the early and late stages of the post-operative period.
Improving cancer care and patient survival is increasingly emphasising on the need to address the long-term impacts of disease and cancer treatments on the clinical, social and emotional realms. Our Department of Oncology has developed over the years a series of proposals aimed at supporting patients and their families who refer to the Breast Unit, ensuring patients’ welfare and accompanying them through their cancer experience.
The multidisciplinarity determined by PDTA makes optimal management in the diagnosis and treatment of cancer patients. In this context, the integration with the pharmacy too, guarantees such multidisciplinarity also for pharmacological treatment. In this way all the patient’s path is standardised, reproducible and traced. The multidisciplinary team within Breast Unit is composed of breast surgeon, oncologist, radiologist, radiotherapist, pathologist, trained nurse and data manager, that represent the core team: they are assisted by plastic surgeon, psychologist, physiatrist, physiotherapist and geneticist. The role of each professional varies depending on the individual case of breast cancer patient and on stage of disease and is tightly integrated with that of other specialists (Figure 2A and 2B).
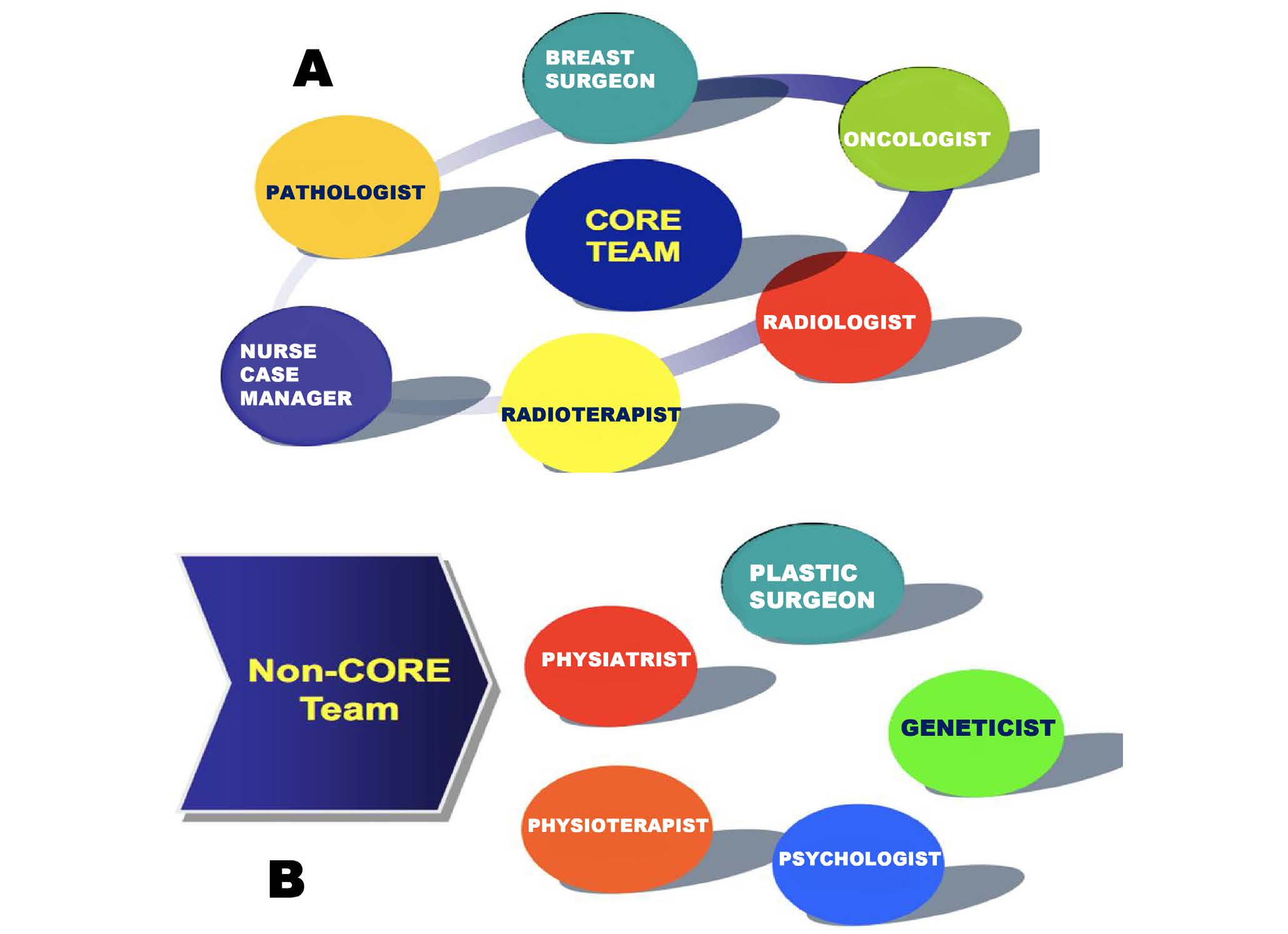
Figure 2: Breast Unit: representation of core team (A) and non-core team (B).
Every week the core team collectively discusses each clinical case, both at the time of clinical suspicion and/or diagnosis and, subsequently, after curative surgery for patients with early stage breast cancer (Figure 3).
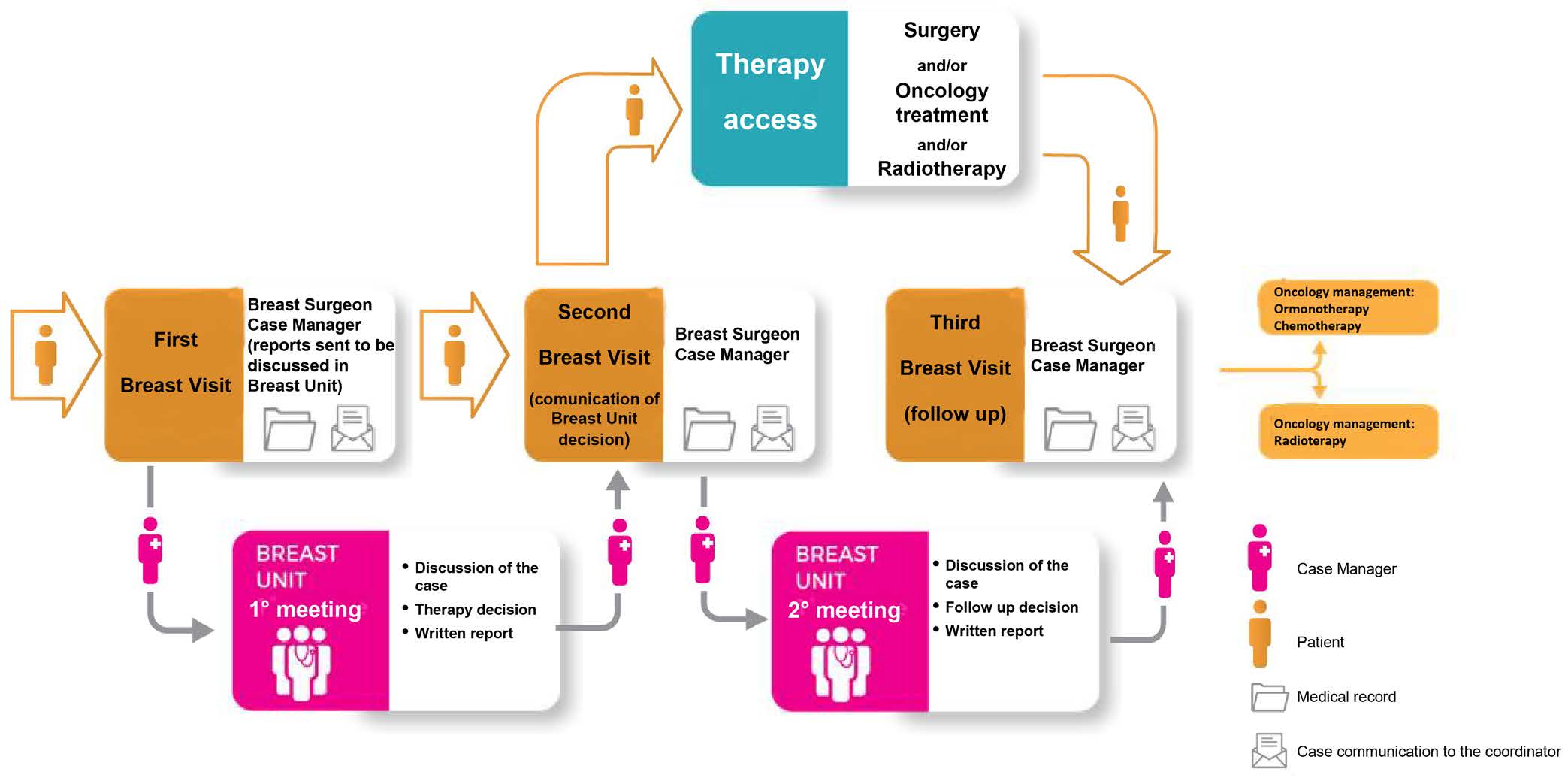
Figure 3: Breast Unit organization.
Furthermore, the Breast Unit employs a coded database and evaluates the quality of care based on predefined indicators used for monitoring PDTA and the activities of the Breast Unit itself.
The monitoring findings may then be evaluated and discussed in individual Breast Units and then in specific regional audits to assess compliance with the guidelines and obtain quality certification.
Molecular tumour board (MTB)
As aforementioned, patients with cancer patients require a multidisciplinary management at different times in the course of the disease from the onset and a shared approach is always the best solution.
In June 2021, the AOU Ospedali Riuniti di Ancona founded a new pathway in the frame of the CORM, setting up the MTB for the first time in Marche region. MTB has been developed on a Web Based Corporate platform, within which Oncologists from different Centers can required an assessment for cancer patients. In details, the MTB aims to:
- Conduct molecular analyses on serological and tissue samples in order to reveal all potential tumour targets; molecular findings will be compared with online databases, to provide specific recommendations for possible treatments, most often off-label.
- Help clinicians in other issues, such as the choice of the most appropriate sample for molecular analysis in relation to the patient’s general clinical condition (histological/cytological sample or liquid biopsy), the type and method of molecular analysis, and the gene panel (large versus small panels), and finally the interpretation of the results obtained, especially in doubtful cases.
- Help health care professionals involved in the management of the cancer patient to translate the complex molecular information into usable data in order to establish the most appropriate treatment for each patient.
Multidisciplinary MTB meetings take place periodically (every two weeks) and represent an opportunity for discussing targeted therapy options for advanced cancer patients, with recent diagnosis (especially for rare neoplasm), or who became resistant to previous therapies. Most decisions are based on information from NGS analysis of tumour DNA obtained from solid or liquid biopsies.
Genomic analysis is performed on the nucleic acids (DNA or RNA) of the tumour, extractable from a histological sample (derived from surgical resection or tumour biopsy) or from circulating tumour cells (liquid biopsy). It is carried out by means of a test based on the NGS technique and analysis of a specific panel of genes, in relation to the indication given by the MTB Team after the discussion of the cases.
The MTB is composed of a default “core” team and other professionals. The “core” team is comprised of a coordinator, secretary, oncologists (including preliminary assessment), pathologist and molecular biologist, geneticist, pharmacist, pharmacologist, data manager, research nurse, case manager, bioethicist, and clinical epidemiologist.
Other specialists included in MTB are: radiologist, interventional radiologist, radiotherapist, surgeon and, possibly, gastroenterologist, pneumologist, or haematologist.
The MTB is activated through a request made on the webbased teleconsultation platform of the CORM by a registered healthcare professional (general practitioner or other specialists). The applicant uploads to the platform the health documents useful for the MTB to take charge of the case. Following the upload, the MTB provides feedback on the multidisciplinary team meeting where the discussion will take place. The participation of the core members of the MTB is always guaranteed at the meetings and they can avail themselves of the constant collaboration of all the consultants needed to complete the clinical assessment of each case.
Within the MTB the cases that can be collectively discussed and shared are the following ones:
- Patients with advanced/metastatic disease who have received a genomic profiling test and who present mutational alterations without immediate and unambiguous clinical classification (rare mutations, presence of co-mutations, etc.) or for which there are no molecularly targeted drugs approved in clinical practice.
- Patients with advanced/metastatic disease and good Performance Status (ECOG 0/1) who have already undergone the standard therapeutic lines and for whom a genomic profiling test with NGS may be indicated.
- Patients with rare diseases orphaned by recognized therapeutic approaches or with few therapeutic options or in rapid progression after standard therapies, with good Performance Status and for whom a genomic profiling test with NGS may be indicated. Patients with “oncogeneaddicted” malignancies not responsive to already available molecular drugs.
At the end of the MTB meeting, the results are summarised and communicated through a specific written feedback (report, shared report or clinical report through the information of CORM platform).
The activity of the Core team members is characterised by multidisciplinarity and multi-professionalism, mutual trust and decision-making convergence, regularity and assiduity of meetings, continuity of contacts, and effective and constant coordination.
CONCLUSION
In recent years, diagnostic and therapeutic innovations have ensured a better survival of cancer patients, so that cancer can be considered a chronic disease and patients need to be fully cared for to improve their quality of life.
In this scenario, there are two ways for providing the best possible care of cancer patients: on the one hand, in recent years, the role of the multidisciplinary approach has become increasingly significant, on the other side the development of precision medicine.
The multidisciplinarity allows observing the patient from several perspectives, ensuring a shorter and more secure approach through constant interaction between the many physicians and specialists.
The complete patient monitoring, the greater understanding of the clinical specificities of the patient, and the advent of genetic diagnostics and targeted therapies have led to the development of precision medicine. Precision medicine in cancer care is based on the use of gene expression technologies, which enables more precise and efficient prediction of personalised therapies best suited for specific patients.
Our Department of Oncology also takes advantage of the important role of multidisciplinary teams through the establishment of PDTA, CORM, MTB, within which there is the possibility of performing NGS-based genomic analysis. It will be significant in the future to be able to implement the use of these practices to provide the best possible personalised care for cancer patients.
Source of Funding
None.
Conflict of Interest
Rossana Berardi is a consultant/advisory board member for Astra Zeneca, Boehringer Ingelheim, Novartis, MSD, Otsuka, Eli-Lilly, Roche. The other authors declare no conflict of interest.
REFERENCES
- Comandone A, Gori S, Nicolis F. CAREGIVER IN ONCOLOGIA. 2021. Available at: https://www.fondazioneaiom.it/wp-content/up-loads/2021/05/2021_ROPI-FondazioneAIOM_FOCUS_Caregiver.pdf. Accessed April 26, 2022.
- Phillips JL, Currow DC. Cancer as a chronic disease. 2010. Available at: https://pubmed.ncbi.nlm.nih.gov/20738055/. Accessed June 21, 2022. DOI: 10.1016/j.colegn.2010.04.007
- Soukup T, Lamb BW, Sevdalis N, Green JSA. Streamlining cancer multidisciplinary team meetings: challenges and solutions. 2020. Available at: https://pubmed.ncbi.nlm.nih.gov/32239992/. Accessed June 21, 2022. DOI: 10.12968/hmed.2020.0024
- Blackwood O, Deb R. Multidisciplinary team approach in breast cancer care: Benefits and challenges. 2020;63:S105–12. Available at: https:// pubmed.ncbi.nlm.nih.gov/32108641/. Accessed June 21, 2022. DOI: 10.4103/IJPM.IJPM_885_19
- Ciemins EL, Brant J, Kersten D, Mullette E, Dickerson D. Why the Interdisciplinary Team Approach Works: Insights from Complexity Science. 2016. Available at: https://pubmed.ncbi.nlm.nih.gov/27104490/. Accessed June 21, 2022. DOI: 10.1089/jpm.2015.0398
- Carle F. Direzione Generale della Programmazione sanitaria. Available at: https://www.salute.gov.it/portale/lea/documenti/pdta/Manuale_PDTA_indicatori_all_1_DPCM_23_07_2018.pdf. Accessed April 26, 2022.
- Ministry of Health Monitoring and evaluation of Diagnostic-Therapeutic Assistance Pathways Methodology for the calculation of indicators. Available at: https://www.salute.gov.it/imgs/C_17_pagineAree_5238_3_file.pdf. Accessed April 26, 2022.
- Schmidt KT, Chau CH, Price DK, Figg WD. Precision Oncology Medicine: The Clinical Relevance of Patient Specific Biomarkers Used to Optimize Cancer Treatment. J Clin Pharmacol 2016;56:1484-1499. DOI: 10.1002/jcph.765
- Tsimberidou AM, Fountzilas E, Nikanjam M, Kurzrock R. Review of Precision Cancer Medicine: Evolution of the Treatment Paradigm. 2020. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC7272286/. Accessed June 21, 2022. DOI: 10.1016/j.ctrv.2020.102019
- Gandamihardja TAK, Soukup T, McInerney S, Green JSA, Sevdalis N. Analysing Breast Cancer Multidisciplinary Patient Management: A Prospective Observational Evaluation of Team Clinical Decision-Making. 2019. Available at: https://pubmed.ncbi.nlm.nih.gov/30382292/. Accessed June 21, 2022. DOI: 10.1007/s00268-018-4815-3
- Yang X, Huang J, Zhu X, Shen K, Zhu J, Chen X. Compliance with multidisciplinary team recommendations and disease outcomes in early breast cancer patients: An analysis of 4501 consecutive patients. 2020. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC7375553/. Accessed June 21, 2022. DOI: 10.1016/j.breast.2020.05.008