INTRODUCTION
Hospital care is evolving at a fast pace, driven by technological progress, demographic changes, and emerging diseases that create more uncertainty and, with it, planning challenges. A hallmark of health care is complexity due to the adaptive, dynamic, and unpredictable nature of health systems around the world. This poses a formidable challenge to decision makers and planners at all levels of health systems. Hospital managers are key actors in health systems and are at the frontline for addressing the increasing burden of diseases (acute, chronic, and communicable).[1] System-wide changes create challenges as the volume of patients needing hospital care is growing,[2] patient expectations are evolving,[3] and patient cases are becoming more complex.[4] Amidst these concerns, “quality” is becoming the guiding principle and key objective for health systems and hospitals.[5]
On the side of solutions, hospital managers have many to choose from; the difficulty lies in deciding what investments need to be made today to maintain and improve quality of care for years to come. In this environment, the potential for quality improvements in hospital care is significant; for example, by investing in patient safety – the pillar of quality – up to 15 percent of hospital spending could be saved by eliminating avoidable harm.[6] If hospitals align these improvements to wider health system objectives, then mutual private and public benefits can be achieved. This is challenging and requires long-view and system-centric models for hospital planning.
HOW TO INVEST: DIAGNOSING THE PROBLEM(S)
Delivering adequate capacity to serve growing patient volumes whilst ensuring high quality care for every patient, within the available resources, is a double challenge. If service expansion is the main concern for any hospital, then volume growth may be the core problem for the given investment period. If quality improvement is the main concern, then management and quality control functions (at existing volumes) may be core. Targeting both dimensions, simultaneously, requires effective planning.
Effective hospital planning requires a diagnosis based on three tenets: (1) the unmet needs of the population, (2) expected demand for care from that population, and (3) resources (financial, workforce and technology) to ensure capacity and quality over the planning period. For each tenet, the volume of cases and quality of services per patient need to be estimated/anticipated. Unmet need is measured by assessing the state of population health and gaps in health system performance; expected demand is based on the expressed (health) needs of a population.[7] Hence, gaps between unmet need and expressed need from the population signal a role for hospitals to provide different services. Resourcing is a function of unmet need and expected demand. Resource use or capacity need is determined by estimating the number of patients who will express their unmet needs and the nature of these cases. For tenet one, planners need to segment the market to determine needs based on meaningful groupings of the population being served.[8] For tenet two, demand and capacity models can be developed using historical service use data, disease burden estimates, and internal knowledge of current capacity.[9] Tenet three is the estimation of capital requirements to meet demand estimates, expressed as human and/or physical capital needs at the hospital level; these will usually be monetised for funding efforts that follow. Prediction remains hard due to the complexity of health systems,[10] nevertheless estimates are needed to guide resource allocation decisions (and improve on them incrementally). The workforce is a key resource that is difficult to secure at short notice, therefore long-term planning is essential.
For planners, these tenets can be used to identify major gaps between the current and future capacity of hospital services. The full range of services should be evaluated using these tenets and pragmatic management methods are needed to categorise the planning efforts by disease area(s), service area(s), or by cost centre(s). A departmental approach can silo efforts, which is why cross-functional managers are needed. Cross-functional managers de-silo planning efforts and create coherent connections across a hospital system, enhancing the quality of information produced during the planning process. The resulting diagnosis integrates problems at a local strategic level, creating the conditions for coherent decision making.
GUIDING PRINCIPLES
The guiding principles of health systems are those in which hospitals also operate; these principles are shaped by health systems’ final goals and intermediate objectives. Quality and value are embedded in these objectives. Hospital management decisions must follow a sound diagnosis of the problem(s),[11] as explained, and investments in human and physical capital should address gaps that are based on this diagnosis. Investments must also align to the guiding principles.
Health systems are guided by their final goals, which aim to improve the health of the populations being served.[12] National health leaders use these aims to set their objectives. In these, health improvement, people-centredness, financial protection, health system efficiency and equity are final goals. These goals should be reflected in those of the government, payers, policy makers, politicians, regulators, and the population. As providers in this system, hospitals are expected to directly contribute to intermediate objectives, which are those that drive achievement of the final ones. Quality encapsulates the intermediate objectives, which include: effectiveness, safety, user-experience, access, efficiency, and equity.
For hospital managers, a guiding principle of “value-based health care” (VBHC) can be used to align planning to the quality improvement efforts across the health system[13]. Value is hard to define, not least of all because it is shaped by “values” which are context-specific; that is, what is valued in one society may be different in another because of different values. Value frameworks that support hospital and system-wide investment in health care are likely to emerge, albeit for now efforts focus on health technology investments rather than the full spectrum of investments and contexts[14,15]. Considering this, hospitals can construct value-based principles based on national interpretations of value, which are themselves linked to international standards. VBHC is a recommended guiding principle for investment because, at a minimum, it reduces short-term, cost-led investment that may be wasteful and contrary to quality improvement,[16,17] which is key to achieving long-term, final goals. Crucially, this principle aligns hospital investments to those of health systems, thereby creating demonstrable alignment between hospitals and the health system; these conditions may support central funding allocation to hospitals (creating new revenue sources) and could lead to new contracts delivered through local or national purchasing processes. In the United States, contract-based initiatives such as readmission reduction programmes that link patient outcomes to hospital payments have shown improvement in value-based activities that benefit both hospitals and health systems.[18] Hospital planners might benefit from co-creating similar programmes in their context, thereby becoming shapers rather than takers in these initiatives.
EFFECTIVE INVESTMENT INVOLVES COHERENT ACTIONS
Guiding principles foster coherent actions over the long-term. These principles provide direction on a long journey into uncharted territory. In hospital care, VBHC investment depends on sound understanding of gaps. The potential to deliver value to the population increases with the size of the gap(s). Thus, incremental improvement against a large gap in high quality care (itself a relative idea) is synonymous with delivering VBHC. Incremental improvement is akin to reducing the performance gap at the hospital and health system level. Coherent actions are needed to achieve this. A strong command of data and the ability to make rational decisions as an organization is at the heart of closing service and performance gaps; for this, the “binocular model” (Figure 1) for long-view hospital planning is needed.
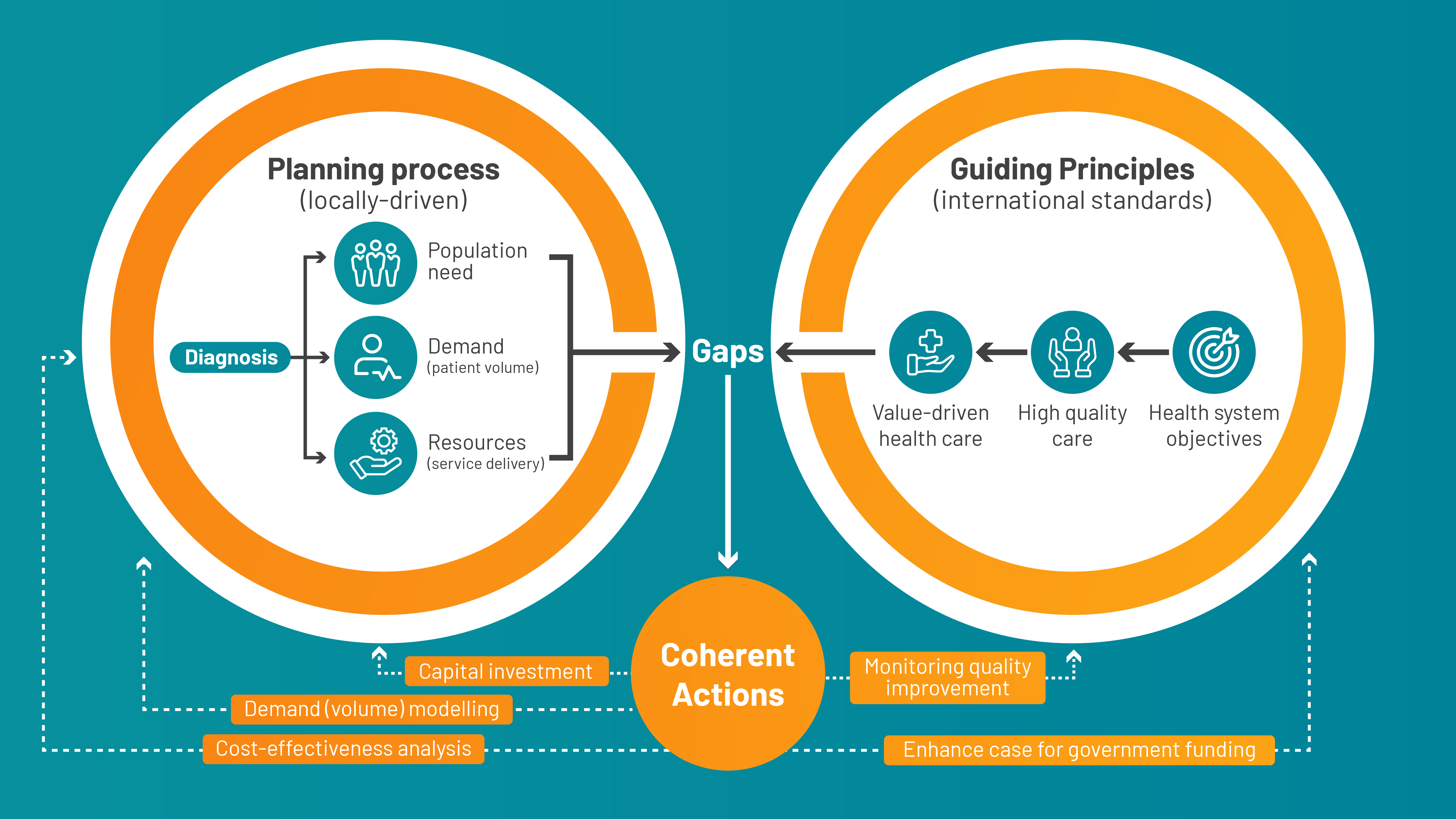
Figure 1. The binocular model is a novel approach to hospital planning that can enhance quality and value in health care. The graphic conveys the need for a sound diagnosis of the current situation (left side) across three tenets/dimensions: the unmet needs of the population, expected demand for care from that population, and resources (financial, workforce and technology). The type and size of gaps in hospital planning are shaped by the guiding principles for health systems (right side). These principles originate in health systems’ final goals and intermediate objectives. Coherent actions must address gaps between standards for high-quality and value-driven health care, and current hospital performance. These actions will feedback into future hospital performance, which is measured against both local targets and international standards. A long/binocular view on planning is essential for incremental improvement.
Given the number of solutions that hospital planners can choose from to improve their performance, there is a need to first invest coherently, then continuously learn from investments. For example, a decision to build more outpatient clinics must be weighed against the potential for the same resources to raise quality by other means, with fewer (opportunity) costs. It could be that existing clinics require less investment to achieve the same quality objectives (and patient volume). To make these decisions, methods rooted in health economics and decision sciences can be used in hospitals.
Health economics is a field concerned with VBHC. Economists developed cost-effectiveness analysis as a method for choosing between alternative technologies, procedures, or care pathways to provide a coherent and transparent means of investing in services. VBHC can be realised if hospitals train or recruit a workforce with these capabilities, hence VBHC starts by investing in human capital. Without these capabilities a long-term value-based strategy cannot be implemented. To be done coherently, it must be stewarded by professionals who possess the requisite analytical skills. Given the rate of technological change in health systems, these skills are increasingly valuable to hospital planners faced with many investment choices and performance gaps to incrementally improve on. Logically, the first investment is the one that can dramatically improve all subsequent hospital investments in human and physical capital.
Value assessment is needed to choose investments wisely. Hospitals should develop capacity for assessing the cost-effectiveness of competing solutions. For example, virtual wards are an alternative to physical wards, having played an important role during the coronavirus pandemic; should hospital managers invest in a virtual hospital or not? What platform should be chosen among the technology platforms available to, for example, maximise the user experience? The investment decision can be made using value assessment methods that account for current and anticipated demand for such services, considering the resource constraints facing the hospital. The fundamental idea is to choose investments in health care delivery that yield the most quality at a cost that the organization is willing-to-pay. Applying this approach across a hospital system should, in aggregate, yield high quality care and reduce waste, albeit expected value can take months or years to manifest given barriers to organizational change.[19] Moreover, health systems face exogenous shocks such as pandemics, natural disasters, and war, which will challenge long-view planning. For this reason, resilience is now a major theme for health system strengthening.[20] The binocular model we propose is an intervention for resilience because, although plans will be disrupted, hospital planners may be better prepared for shocks using this investment approach.[21]
Future research should measure the extent to which system-wide outcomes are achieved using the binocular model. This extends to capturing potential unintended consequences of this planning approach and adapting the model for different contexts based on evidence.
THE CASE OF INTEGRATED CARE
Integrated care is an increasingly accepted organizing principle in large health systems[22] and there are major implications for hospitals. A seamless interface between providers of health and health care is crucial to health system resilience and, therefore, increasingly relevant to hospital planners in the post-pandemic world. Integrated care moves beyond value within a single-centre and considers how linking care between organisations can deliver VBHC. For hospital managers, this means that unmet need, expected demand, and resourcing must be analysed beyond the traditional bounds of the hospital system. The guiding principles for integrating care mirror those of the health system at-large,[22] albeit high-income settings are yet to fully realise the benefits of this move, possibly because organizational changes take years to produce cost and quality improvements.[23]
The implication of this is more collaboration and increased use of shared funding models between primary care providers and hospitals because diseases will need to be diagnosed, treated, and managed in several settings. In effect, value-driven investment may need to be made elsewhere. Therefore, technology and data (sharing) are required for integration to occur.[24] Hospitals that invest in the most cost-effective care delivery models may reap the benefits of this change first by reducing waste and producing high-quality care that is attractive to public insurers and patients. By aligning hospital plans to integrated care models, long-term benefits from accessing larger funding sources can be realised. This moves hospitals that currently operate as private entities into quasi-public providers with diversified revenue streams and greater means to innovate.
CONCLUSION
The changing role of hospitals in health systems necessitates change in capabilities, exemplified by the need to invest in decision science professionals. Hospital planners need to diagnose problems, establish guiding principles that align to international standards, and invest coherently using the three tenets given in this article. Innovative planning should align hospital investments to health system goals, which also capture value to the many stakeholders involved. Hospital managers and medical professionals can use the “binocular model” to support their efforts. The planning process we describe is system-centric and adopts a long-view; uncertainties will be navigated in reality that will challenge the idealised approach proposed. We argue that this approach is essential because hospitals and health systems must adopt methods that improve resilience to shocks. In doing so, hospitals and the populations they serve will benefit.
DECLARATIONS
Conflict of interest
Salman Rawaf is the Editorial Board Member of the journal. The article was subject to the journal’s standard procedures, with peer review handled independently of the editor and the affiliated research groups.
REFERENCES
- 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. DOI: 10.1016/S0140-6736(20)30925-9 PMID: 33069326
- Xiao Y, Qiu QM, Huang YX, Zhu SY. Patients gather in large hospitals: the current situation of Chinese hospitals and the direction of medical reform. Postgrad Med J. 2022;98(1166):e43. DOI: 10.1136/postgradmedj-2021-140147 PMID: 33879544
- Larson E, Sharma J, Bohren MA, Tunçalp Ö. When the patient is the expert: measuring patient experience and satisfaction with care. Bull World Health Organ. 2019;97(8):563–569. DOI: 10.2471/BLT.18.225201 PMID: 31384074
- Tonelli M, Wiebe N, Manns BJ, Klarenbach SW, James MT, Ravani P, et al. Comparison of the Complexity of Patients Seen by Different Medical Subspecialists in a Universal Health Care System. JAMA Netw Open. 2018;1(7):e184852. DOI: 10.1001/jamanetworkopen.2018.4852
- Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. Lancet Glob Health. 2018;6(11):e1196–e1252. DOI: 10.1016/s2214-109x(18)30386-3
- Slawomirski L, Auraaen A, Klazinga NS. The economics of patient safety. OECD Publishing; 2017. Accessed December 29, 2022. https://www.oecd.org/els/health-systems/The-economics-of-patient-safety-March-2017.pdf
- Bradshaw J. Taxonomy of social need. In: McLachlan G, ed. Problems and progress in medical care : essays on current research. 7th ed. Oxford University Press; 1972: 71–82. DOI: 10.1017/s004727940005011x
- Nnoaham KE, Cann KF. Can cluster analyses of linked healthcare data identify unique population segments in a general practice-registered population? BMC Public Health. 2020;20(1):798. DOI: 10.1186/s12889-020-08930-z
- Demir E, Gunal MM, Southern D. Demand and capacity modelling for acute services using discrete event simulation. Health Syst. 2017;6(1):33–40. DOI: 10.1057/hs.2016.1
- Greenhalgh T, Papoutsi C. Studying complexity in health services research: desperately seeking an overdue paradigm shift. BMC Med. 2018;16(1):95. DOI: 10.1186/s12916-018-1089-4 PMID: 29921272
- Rumelt R. The perils of bad strategy. McKinsey Q. 2011:30–39.
- World Health Organization, European Observatory on Health Systems and Policies, Papanicolas, Irene, Rajan, Dheepa, et al. Health system performance assessment: a framework for policy analysis. World Health Organization; 2022. DOI: 10.1136/bmjopen-2018-022345
- Smith PC, Sagan A, Siciliani L, Panteli D, McKee M, Soucat A, et al. Building on value-based health care: Towards a health system perspective. 2020. Europe PMC website. Published April 13, 2021. Accessed December 28, 2022. http://europepmc.org/abstract/MED/33844486 DOI: 10.2471/blt.10.077339
- Pearson SD. The ICER Value Framework: Integrating Cost Effectiveness and Affordability in the Assessment of Health Care Value. Value Health. 2018;21(3):258–265. DOI: 10.1016/j.jval.2017.12.017 PMID: 29566831
- Neumann PJ, Garrison LP, Willke RJ. The History and Future of the ISPOR Value Flower: Addressing Limitations of Conventional Cost-Effectiveness Analysis. Value Health. 2022;25(4):558–565. DOI: 10.1016/j.jval.2022.01.010 PMID: 35279370
- OECD. Tackling Wasteful Spending on Health. OECD Publishing; 2017. Accessed December 22, 2022. https://doi.org/10.1787/9789264266414-en
- Chalkidou K, Appleby J. Eliminating waste in healthcare spending. BMJ. 2017;356:j570. DOI: 10.1136/bmj.j570 PMID: 28174162
- Ryan AM, Krinsky S, Adler-Milstein J, Damberg CL, Maurer KA, Hollingsworth JM. Association Between Hospitals’ Engagement in Value-Based Reforms and Readmission Reduction in the Hospital Readmission Reduction Program. JAMA Intern Med. 2017;177(6):862–868. DOI: 10.1001/jamainternmed.2017.0518 PMID: 28395006
- Morris ZS, Wooding S, Grant J. The answer is 17 years, what is the question: understanding time lags in translational research. J R Soc Med. 2011;104(12):510–520. DOI: 10.1258/jrsm.2011.110180 PMID: 22179294
- Ghebreyesus TA, Jakab Z, Ryan MJ, Mahjour J, Dalil S, Chungong S, et al. WHO recommendations for resilient health systems. Bull World Health Organ. 2022;100(4):240–240A. DOI: 10.2471/blt.22.287843
- Haldane V, de Foo C, Abdalla SM, Jung AS, Tan M, Wu S, et al. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med. 2021;27(6):964–980. DOI: 10.1038/s41591-021-01381-y
- Yip W, Fu H, Chen AT, Zhai T, Jian W, Xu R, et al. 10 years of health-care reform in China: progress and gaps in Universal Health Coverage. Lancet. 2019;394(10204):1192–1204. DOI: 10.1016/s0140-6736(19)32136-1
- Baxter S, Johnson M, Chambers D, Sutton A, Goyder E, Booth A. The effects of integrated care: a systematic review of UK and international evidence. BMC Health Serv Res. 2018;18(1):350. DOI: 10.1186/s12913-018-3161-3 PMID: 29747651
- Cresswell KM, Mozaffar H, Lee L, Williams R, Sheikh A. Safety risks associated with the lack of integration and interfacing of hospital health information technologies: a qualitative study of hospital electronic prescribing systems in England. BMJ Qual Saf. 2017;26(7):530–541. DOI: 10.1136/bmjqs-2015-004925 PMID: 27037303